The WHO likes dividing its operations into clusters and pillars. For Ebola there are 6 pillars supporting the emergency response:
1) Isolation of patients - this is the main role of our expensive Ebola Treatment Centres - more quarantine centres than treatment centres
2) Safe burials - Ebola is at its most dangerous in the final stages and after death - a clever evolutionary trick
3) Awareness raising - changing behaviours of an entire population - to notify cases, to wash hands and stop touching
4) Alert and surveillance - basic epidemiology to help inform the who, where and when of Ebola and to monitor trends.
5) Contact tracing - this is always low down for infection control in Africa (eg TB where it always happens in the UK but rarely happens in Africa), but for Ebola the efforts have been ramped up
6) Health access for non-Ebola cases. It is this pillar that we delve into today.
At Bo we are being taught by MSF how to run an Ebola Centre and some of the many lessons they have learnt. MSF have had 25 of their health workers infected with Ebola - 22 national and 3 international. Most of these are dead.
Today we deal with how to handle fevers in staff. There is a bit of tramline thinking when it comes to fevers and it’s important not to forget the other common causes (malaria, Lassa etc). However, what MSF have found is that staff are cautious about coming forward.
They have seen at first hand the suffering and mostly fatal outcomes of the patients on the wards, and this is the last place they want to get sent to. So they cover up and they self-medicate, all the while increasing the risk of spread to their colleagues.
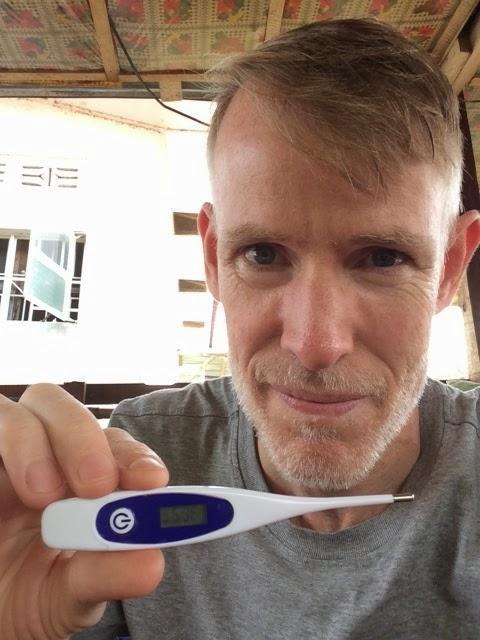
So a proactive approach has been adopted. All staff have thermometers and do thrice daily temperatures (must remember to start doing mine). The cheap Chinese laser thermometers are not trusted, so all staff need to measure their axillary temperature before they leave home, and then on arrival at the Ebola Centre.
They are only let in to the Ebola Centre when they show the reading to the security guard. Bed nets and antimalarials are provided to all staff now in order to reduce the chance of malaria and the fear that a malaria fever will bring (all fevers are Ebola until proven otherwise).
Personal hygiene kits are given to everyone for use at home. The no-touching rule is easy to enforce for international staff (two MSF staff were found to be ‘intimately touching’ and sent home on the next plane out of Freetown) - they are only in the country for a limited period of time. But what do you do for national staff? They have wives and husbands and children. The no-touching rule is limited to non-family members for these long-term heroes.
If the staff are suspected to have Ebola then it’s straight to admission and isolation (a grim destination). For international staff there is a 48 hour escape rule - if you think you have been exposed then you have a 48 window to travel back to your country before you are at risk of infection. Any possible exposure and you pack your bag, get taken to the airport and catch the next plane out.
But what happens if it’s not Ebola? What happens if you have suspected appendicitis? The hospitals have become plague villages, transmission centres for the disease. If you can persuade the staff member to go there, then it’s unlikely anyone will go near you. Too many surgeons have died from operating on Ebola patients and their surviving colleagues will not enter the same room as a suspected case let alone wield a scalpel.
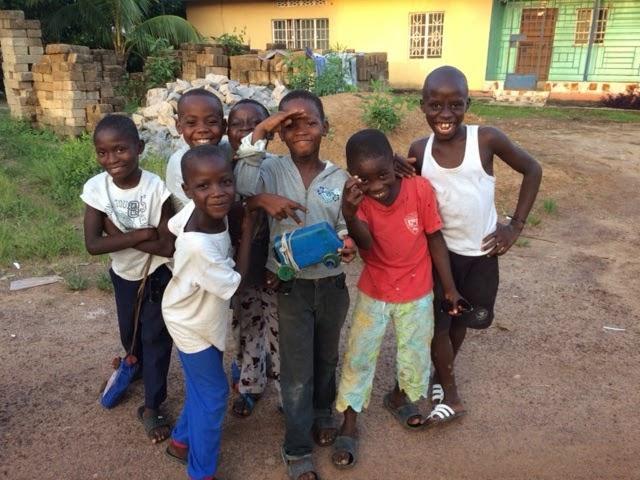
I have made friends with the children living next to my guest house in Bo. They are always hanging around as their school closed months ago. Now when they see me returning they rush out full of joy and excitement and hug me, grabbing my hands and dancing with me. What a terrible dilemma - I can’t tell them to stay away. I join in the excitement and cover up my discomfort. I ask Joanna, age 6, what she knows about Ebola.
“Never touch anyone sick, wash your hands in chlorine water, if you suspect person has Ebola then call 117, and always do what the Well Body Ministry tells you’ she recites in a sing song voice. I like the last bit - always obeying what the Ministry of Health tells you. I’ll bring this back as a suggestion for the NHS.
Today we get handed over the keys for our Ebola Centre from the Royal Engineers. 17 truck-loads of medical supplies has left Freetown. We have three days to unload them and to fit out our hospital, but this is for our logisticians. Tomorrow I get my first clinical experience in the red zone.
MORE BLOG POSTS FROM PROFESSOR JOHN WRIGHT



Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereComments are closed on this article